How Long Can Silicone Oil Remain in the Eye
- Original article
- Open Access
- Published:
Timing and outcomes afterwards silicone oil removal in proliferative vitreoretinopathy: a retrospective clinical series
International Journal of Retina and Vitreous volume 1, Article number:ii (2015) Cite this article
Abstruse
Objective
To evaluate anatomical and functional outcomes after silicone oil extraction in patients with retinal detachment and proliferative vitreoretinopathy in an middle care referral center in Joinville, SC, southern Brazil.
Methods
Retrospective, noncomparative study of patients with retinal detachment and posterior proliferative vitreoretinopathy followed upwardly after silicone oil removal. Prophylactic 360-degree peripheral laser photocoagulation was performed ane to iii months earlier silicone oil extraction. Patients with cataract underwent a combined clear corneal phacoemulsification with intraocular lens implantation in the same procedure. Anatomical outcomes were related to the duration of silicone oil tamponade and the surgical process performed. Functional outcomes were divided into three categories (stability, worsening, or improvement) co-ordinate to visual acuity variation before the surgery and at the last follow-up visit.
Results
Fifty-three patients were followed upwardly for a mean menstruum of 1,262 days.
14 eyes (26.4%) underwent cataract surgery combined with silicone oil extraction. Forty-eight eyes (ninety.five%) had attached retina at the last follow-up examination. Time of intraocular tamponade and association of phacoemulsification with silicone oil extraction were not considered as risk factors for retinal redetachment. Xx-three cases (43.4%) showed visual acuity improvement, whereas 11 cases (20.8%) were stable and 19 cases (35.8%) showed visual acuity worsening. 5 patients with fastened retina had unexplained optic disc atrophy.
Decision
Most patients had good anatomical and visual outcomes later on silicone oil extraction. Rubber 360-degree laser retinopexy may accept led to favorable outcomes. Benefits of silicone oil extraction and the associated risks of complications due to a new surgical process must be carefully evaluated before surgical indication.
Background
Proliferative vitreoretinopathy (PVR) is an of import complication of rhegmatogenous retinal disengagement and its handling requires a long-acting endotamponade, such as silicone oil, to reduce the rate of recurrent retinal detachment [1,ii].
To avoid long-term complications due to the presence of silicone oil inside the centre, such as cataract, glaucoma and ceratopathy, its removal is usually necessary. Even so, after silicone oil extraction, recurrence of PVR and consequently retinal redetachment can occur. It is by and large associated with balance vitreoretinal traction at the vitreous base of operations [three,4]; some other factors may as well contribute to unfavorable outcomes, like intra and postoperative inflammation, intraoperative bleeding, retinal pigment epithelium exposure, retinectomy and extended duration of the surgical procedure.
Every bit suggested by some authors, a condom 360-degree laser retinopexy prior to silicone oil extraction may aid to reduce retinal redetachment rates [5-7]. Additionally, in spite of a permanent attached retina, some patients may have unexplained vision loss after silicone oil extraction [i,3-7].
The objective of the present report is to evaluate anatomical and functional outcomes afterwards silicone oil removal in patients with retinal detachment and proliferative vitreoretinopathy in an heart care referral center in Joinville, SC, southern Brazil.
Methods
A retrospective, noncomparative clinical series of patients with rhegmatogenous retinal detachment and posterior PVR form A, B, C1, C2, C3, D1 and D2 examined after silicone oil extraction. Surgical interventions were performed between January 1997 and February 2013. The patients were examined and operated on past the aforementioned surgeon (MJN).
The initial operative procedure consisted of twenty-approximate pars plana vitrectomy, 360-degree scleral buckle, laser endophotocoagulation surrounding retinal tears, and infusion of 5000-centistoke silicone oil (Ophthalmos®, São Paulo, SP) into the vitreous cavity (Effigy 1). Prophylactic 360-caste peripheral laser photocoagulation was performed one to three months before silicone oil extraction. Laser spots were delivered to the scleral buckle surface area in two or three rows via slit lamp.
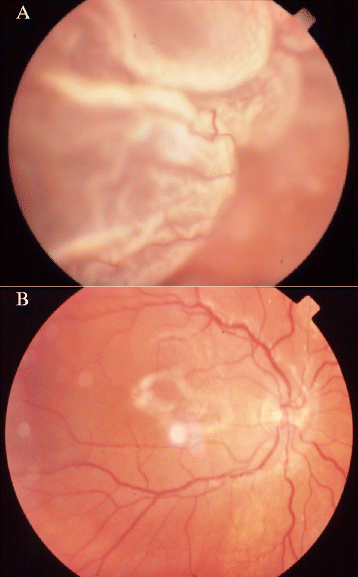
Inicial operative procedure: rhegmatogenous retinal detachment and grade C posterior proliferative vitreoretinopathy (A) and postoperative upshot afterward silicone oil infusion (B).
Silicone oil was extracted between 6 weeks and 12 months after the initial procedure through a standard two-port pars plana surgery. If there was cataract, a combined clear corneal incision phacoemulsification and intraocular lens (IOL) implantation was performed. During follow-upwardly catamenia, logMAR best-corrected visual acuity (BCVA), intraocular pressure (IOP), slit-lamp biomicroscopy, indirect and slit-lamp ophthalmoscopy were registered.
Functional outcomes were divided into three categories. Patients who had a terminal logMAR BCVA showing a 0.1-variation compared to the baseline BCVA were considered stabilized; a visual acuity variation was significant if the difference between baseline and terminal BCVA was 0.2 logMAR. A severe visual worsening was registered if there was a BCVA reduction of 0.3 logMAR or more.
Statistical analysis was performed using STATA version 12.0 (Texas USA). Categorical variables were expressed past frequencies and percentages and the continuous variables were expressed through means and standard divergence, with a confidence interval of 95%. The Student's t-test was used to evaluate relation between hateful period of silicone oil tamponade and retinal detachment also equally to compare visual acuity means before and after silicone oil removal. Pearson's Chi-square test, or the Fischer exact examination, was used to assess causality of using the combined process (silicone oil removal, phacoemulsification and IOL implantation) with retinal re-detachment cases, and as well correlate it with terminal visual vigil. Significance level of 5% was accepted to reject the cypher hypothesis.
The informed consent to participate in the written report was obtained from each patient. Hospital Municipal São José's ethical commission, Joinville – Santa Catarina, Brazil, approved the research according to the projection number: 240.558.
Results
Fifty-three eyes of 53 patients were included; thirty-three (62%) patients were male; mean age was 52.7 years (range 16–79 years). According to PVR classification, iii.8% (ii/53) of the patients were grade A PVR; five.6% (3/53) class B PVR; 32.ane% (17/53) class C1 PVR; 18.nine% (ten/53) course C2 PVR; 5.6% (three/53) class C3 PVR; 1.9% (i/53) grade D1 PVR and ane.9% (1/53) class D2 PVR; thirty.2% (16/53) of the patients had no classifying register. Follow-up varied from 256 days to 4,421 days (mean ane,262 + −944 days). The median fourth dimension of silicone oil extraction was 196 days after its placement. The mean intraocular force per unit area was 15.6 + −7.4 before and 14.8 + −6.2 after silicone oil removal. Phacoemulsification with IOL implantation was combined with silicone oil removal in 14 eyes (26.4%) (Figure 2A).

Anatomical results afterward silicone oil removal and comparing betwixt single and combined procedure with phacoemulsification.
Forty-eight (90.5%) patients had attached retina at the last follow-upwardly visit (Effigy 2B). The mean period of silicone oil elapsing in the vitreous cavity was 228 + −152 and 275 + −265 days in cases with and without redetachment, respectively. There was no association between duration of intraocular silicone oil and risk for retinal redetachment (p = 0.6997). The charge per unit of retinal redetachment in patients submitted to phacoemulsification combined with silicone oil extraction was 21.4% (Effigy 2C), which represented 60% of all the redetachment cases (Figure 2D), but not statiscally significant (p = 0.0735).
Xx-three patients (43.iv%) showed BCVA improvement, eleven patients (20.8%) were stabilized and nineteen patients (35.eight%) had a BVCA worsening. Hateful preoperative and postoperative values of BCVA were 0.95 logMAR (Snellen = 20/160) and 1.01 logMAR (Snellen = twenty/200) respectively (Figure iii). Severe visual worsening was observed in 15 patients (28.3%), of whom five had unexplained optic disc atrophy.

Comparison of BCVA betwixt preoperative examination and last follow-upward assessment.
Combined phacoemulsification with intraocular lens implant and removal of silicone oil did non influence the final visual acuity when compared to the isolated extraction of silicone oil (p = 0.426). In improver, BCVA worsening could not exist directly associated with silicone oil removal (p = 0.6598).
Give-and-take
Several factors may be related to anatomic and functional outcomes afterwards silicone oil extraction in PVR cases. In this study, the relation betwixt duration of silicone oil tamponade and incidence of retinal redetachment was non established. In the literature, while some authors did not consider the timing of silicone oil removal as a take chances factor for anatomic success rate [4,8,9], others observed that shorter tamponade elapsing had lower attachment rate than longer tamponade duration [10,11].
The association of encircling buckle and peripheral laser photocoagulation prior to silicone oil extraction has been previously reported as safe and advantageous [nine,12-15]. A 360-degrees laser performed previously to surgery may better peripheral chorioretinal adhesion and avoid retinal redetachment in spite of residual vitreous base traction [3,7,16].
Compared to other studies (Table i), the present report showed a low redetachment rate (9.five%) afterwards silicone oil extraction. This may exist due to improved surgical management of complicated retinal detachments in the terminal years, especially adequate vitreous removal with the use of wide-field viewing systems [7,12].
A combined surgery, with longer duration and more than intense inflammation, may predispose to postoperative PVR and retinal redetachment [2]. The present study showed a higher rate of retinal detachment recurrence in optics submitted to silicone oil extraction associated with cataract surgery than eyes that had just silicone oil removal (21.four% vs. 5.1%); withal, this result was non statistically significant (p = 0.0735).
Functional outcomes were not fully correlated with anatomical outcomes. To appointment, there is no definite explanation for vision loss or optic atrophy after silicone oil extraction. A long-term and close contact of silicone oil with the retina may cause toxicity; abnormal potassium exchanges and dysfunction of cardinal Müller cells may as well explain a shallow foveal depression and vision loss [13-15].
Likewise surgical intervention, new types of treatment for PVR are being tested in clinical trials. Several studies have been performed, including employ of many drugs, such every bit daunorubicin, corticosteroids, 5-fluorouracil, heparin and colchicine [17-21]. All the same, PVR is still a claiming and continues to be the most common crusade of surgical failure following retinal detachment surgery.
The main limitation of the nowadays written report is its retrospective and noncomparative design. Considering of the patients' records were not standardized, some complementary data, such as assay of macular optic coherence tomography and visual field, could non exist included. The size of the sample may likewise take influenced the results; a higher number of treated eyes could permit other comparisons and demonstrate significant differences between the outcomes.
Every bit described in other reports, this study shows how critical is the dilemma concerning treatment of complex rhegmatogenous retinal detachment. Silicone oil removal provided favorable anatomical and functional results in the majority of the operated eyes and prophylactic peripheral laser retinopexy may have contributed to this. However, some eyes developed unexplained vision loss after silicone oil extraction and there was as well a trend to retinal redetachment when silicone oil removal was combined with phacoemulsification and intraocular lens placement.
Conclusion
In summary, depression disengagement rate may be due to improved surgical management of complicated retinal detachments and besides to prophylactic 360- degree retinopexy. Surgeons must be aware of adverse results associated with silicone oil removal. Benefits of silicone oil extraction must exist outweighed against its extended elapsing in the eye and the possibility of complications subsequently a new surgical procedure.
Abbreviations
- PVR:
-
Proliferative vitreoretinopathy
- IOL:
-
Intraocular lens
- BCVA:
-
All-time-corrected visual acuity
References
-
Falkner CI, Binder S, Kruger A. Outcome after silicone oil removal. Br J Ophthalmol. 2001;85(xi):1324–vii.
-
Ryan SJ. The pathophysiology of proliferative vitreoretinopathy in its management. Am J Ophthalmol. 1985;100(1):188–93.
-
Jain P, Napgal M, Videkar R, Napgal One thousand, Patil A: Evaluation of possible gamble factors for retinal re-disengagement after silicone oil removal. In: AIOC, Retina/Vitreous session – IV. 2010:655–half dozen.
-
Jonas JB, Knor HL, Rank RM, Budde WM. Retinal redetachment subsequently removal of intraocular silicone oil tamponade. Br J Ophthalmol. 2001;85(10):1203–7.
-
Hutton LW, Azen PS, Blumenkranz SM, Lai MY, McCuen BW, Han DP, et al. The effects of silicone oil removal. Silicone study study half-dozen. Arch Ophthalmol. 1994;112(6):778–85.
-
Steel DH, Weir P, James CR. Silicone assisted, argon laser confinement of recurrent proliferative vitreoretinopathy relates retinal detachment: a technique to allow silicone oil removal in problem eyes. Br J Ophthalmol. 1997;81(ix):765–seventy.
-
Tufail A, Schwartz SD, Gregor ZJ: Prophylactic argon light amplification by stimulated emission of radiation retinopexy prior to removal of silicone oil: a pilot study. Eye (Lond).1997;11 (Pt iii):328–30.
-
Lam RF, Cheung BTO, Yuen CYF, Wong D, Lam DSC, Lai WW. Retinal redetachment after silicone oil removal in proliferative vitreoretinopathy: a prognostic factor analysis. Am J Ophthalmol. 2008;145(3):527–33.
-
Nagpal MP, Videkar RP, Nagpal KM. Factors having implications on reretinal detachments after silicone oil removal. Indian J Ophthalmol. 2012;60(half dozen):517–20.
-
Tan HS, Dell'omo R, Mura M. Silicone oil removal after rhegmatogenous retinal disengagement: comparing techniques. Heart (Lond). 2012;26(three):444–7.
-
Scholda C, Egger South, Lakits A, Walch K, von Eckardstein E, Biowski R. Retinal detachment after silicone oil tamponade. Acta Ophtalmol Scand. 2000;78(2):182–6.
-
Laidlaw DA, Karina N, Bunce C, Aylward GW, Gregor ZJ. Is condom 360-degree light amplification by stimulated emission of radiation retinopexy protective? risk factors for retinal redetachment after removal of silicone oil. Ophthalmology. 2002;109(one):53–8.
-
Cazabon S, Groenewald C, Pearce IA, Wong D. Visual loss following removal of intraocular silicone oil. Br J Ophthalmol. 2005;89(7):799–802.
-
Williams PD, Fuller CG, Scott IU, Fuller DG, Flynn HW. Vision loss associates with the use and removal of intraocular silicone oil. Clin Ophthalmol. 2008;2(4):955–ix.
-
Jain North, McCuen 2nd BW, Mruthyunjaya P. Unanticipated vision loss after pars plana vitrectomy. Surv Ophthalmol. 2012;57(2):91–104.
-
Avitabile T, Longo A, Lentini G, Reibaldi A. Retinal detachment afterward silicone oil removal is prevented by 360 degrees light amplification by stimulated emission of radiation handling. Br J Ophthalmol. 2008;92:1479–82.
-
Sunday JK, Arroyo JG. Adjunctive therapies for proliferative vitreoretinopathy. Int Ophthalmol Clin. 2004;44(three):1–ten.
-
Wiedemann P, Hilgers RD, Bauer P, Heimann K, Daunomycin Study Grouping. Adjunctive daunorubicin in the treatment of proliferative vitreoretinopathy: results of a multicenter clinical trial. Am J Ophthalmol. 1998;126(iv):550–9.
-
Shinohara K, Tanaka Chiliad, Sakuma T, Kobayashi Y. Efficacy of daunorubicin encapsulated in liposome for the handling of proliferative vitreoretinopathy. Ophthalmic Surg Lasers Imaging. 2003;34(four):299–305.
-
Asaria RH, Kon CH, Bunce C, Charteris DG, Wong D, Khaw PT, et al. Adjuvant 5-fluorouracil and heparin prevents proliferative vitreoretinopathy: results from a randomized, double-blind, controlled clinical trial. Ophthalmology. 2001;108(seven):1179–83.
-
Wickham 50, Bunce C, Wong D, McGurn D, Charteris DG. Randomized controlled trial of combined 5-Fluorouracil and depression-molecular-weight heparin in the direction of unselected rhegmatogenous retinal detachments undergoing main vitrectomy. Ophthalmology. 2007;114(4):698–704.
-
Bassat IB, Desatnik H, Alhalel A, Treister G, Moisseiev J. Reduced rate of retinal detachment following silicone oil removal. Retina. 2000;20(six):597–603.
-
Flaxel CJ, Mitchell SM, Aylward GW. Visual consequence afterward silicone oil removal and recurrent retinal detachment repair. Heart. 2000;14:834–8.
-
Assi A, Woodruff S, Gotzaridis E, Bunce C, Sullivan P. Combined phacoemulsification and transpupillary drainage of silicone oil: results and complications. Br J Ophthalmol. 2001;85(8):942–5.
-
Jiang F, Krause M, Ruprecht KW, Hille Thousand: Management and results of retinal detachment subsequently silicone oil removal. Ophthalmologica. 2002 Sep-October;216(5):341–5.
-
Unlu Northward, Kocaoglan H, Acar MA, Sargin M, Aslan BS, Duman Southward. Outcome of complex retinal disengagement surgery after silicone oil removal. Int Ophthalmol. 2004;25(1):33–half dozen.
-
27. Scott IU, Flynn Jr HW, Murray TG, Smiddy WE, Davis JL, Feuer WJ: Outcomes of complex retinal disengagement repair using 1000- vs 5000- centistoke silicone oil. Arch Ophthalmol. 2005 Apr;123(4):473–8.
-
Soheilian M, Mazareei M, Mohammadpour Thousand, Rahmani B: Comparing of silicon oil removal with various viscosities later circuitous retinal detachment surgery. BMC Ophthalmol. 2006 May; 31;6:21.
Author information
Affiliations
Respective writer
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
RLPT: conception and design, acquisition, assay and interpretation of information; involved in drafting the manuscript and its revising. MJN: formulation, design, contributed in drafting, responsible for critical revision and has given last approval of the version to be published. FAJN: design, acquisition and estimation of data. FJN: conception, pattern and revising. CACO: statistical analysis and estimation of data. All authors read and approved the final manuscript.
Rights and permissions
This is an Open Access commodity distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/cipher/1.0/) applies to the data fabricated bachelor in this commodity, unless otherwise stated.
Reprints and Permissions
About this article
Cite this commodity
Tavares, R.L.D., Nóbrega, M.J., Nóbrega, F.A.J. et al. Timing and outcomes afterwards silicone oil removal in proliferative vitreoretinopathy: a retrospective clinical series. Int J Retin Vitr 1, 2 (2015). https://doi.org/10.1186/s40942-015-0002-y
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s40942-015-0002-y
Keywords
- Retinal detachment
- Silicone oil
- Proliferative vitreoretinopathy
Source: https://journalretinavitreous.biomedcentral.com/articles/10.1186/s40942-015-0002-y
0 Response to "How Long Can Silicone Oil Remain in the Eye"
Post a Comment